On 30th Aug 2016, MOH and Clinical advisory group on Zika and pregnancy release guidelines for pregnant women. The guidelines also include frequently asked questions about Zika and pregnancy.
It is understood that pregnant women's partners should also take precaution as Zika can be sexually transmitted. This may be the reason why pregnant women should go for test as stated below if their partner shows symptoms of Zika.
Below we reproduce the guidelines and FAQ for your information. You may wish to visit https://www.moh.gov.sg for the latest update on Zika and pregnancy.
The full article can be found at https://www.moh.gov.sg/content/moh_web/home/pressRoom/pressRoomItemRelease/2016/moh-and-clinical-advisory-group-on-zika-and-pregnancy-provide-gu.html
MOH and clinical advisory group on zika and pregnancy provide guidelines for pregnant women
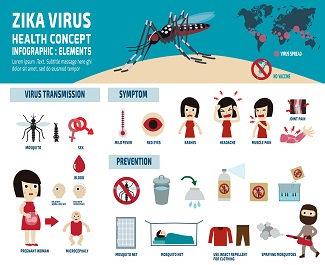
The Ministry of Health (MOH) and the Clinical Advisory Group (CAG) on Zika and Pregnancy advise all pregnant women in Singapore with symptoms of Zika (fever and rash and other symptoms such as red eyes or joint pain), as well as those (with or without symptoms) with male partners who are Zika-positive, to be tested for Zika virus infection. This is regardless of whether they have been to Zika-affected areas.
2. Testing is not routinely recommended for other pregnant women who do not have symptoms of Zika and whose male partners are not Zika-positive.
3. Testing for pregnant women as referred by their doctors, and who meet these criteria, is free at the public healthcare institutions. This is no different from the current practice for Zika testing for those with symptoms and who live, work or study in a Zika-affected area.
4. The clinical guidelines have been updated following the localised community spread of Zika virus infection in the Aljunied Crescent/ Sims Drive area. They are in line with the World Health Organization (WHO)’s current guidelines. The guidelines are being shared with obstetricians and gynaecologists (O&G), and neonatology and paediatric specialists in our Public Hospitals, as well as all polyclinics and general practitioners.
5. MOH’s CAG on Zika and Pregnancy is led by Professor Arijit Biswas, Clinical Director & Senior Consultant, Department of Obstetrics & Gynaecology, National University Hospital, and consists of experts in obstetrics and gynaecology, paediatrics, infectious diseases, and laboratory medicine. Their role is to review the latest information on Zika virus infection and pregnancy, and advise on the development of clinical management protocols for women who may have been exposed to Zika, or have confirmed Zika virus infection. The CAG had met on 30 August 2016 to review and update the guidelines in light of the latest Zika situation in Singapore[1].
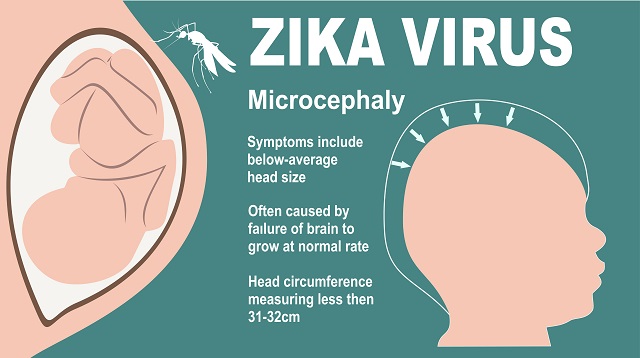
Microcephaly
6. While there is currently no evidence that women are more likely to get Zika virus infection, the consequences can be more serious if a pregnant woman is infected, as Zika virus infection can cause microcephaly in the unborn foetus of pregnant women.
7. Microcephaly is a congenital condition in which the head size is much smaller than usual for a baby of the same age, race and sex. Microcephaly can be caused by a variety of genetic and environmental factors, such as Down Syndrome, exposure to drugs, alcohol or other toxins in the womb, rubella and a few other infections during pregnancy. There is no specific treatment for this condition.
Care for Pregnant Women
8. Pregnant women who do not have any symptoms of Zika will be monitored for the duration of their pregnancy as part of their routine prenatal care. For those who are concerned, their O&G doctor may offer regular foetal ultrasounds to further check on the foetus’ health.
9. If a pregnant patient is confirmed to have Zika infection, she will be referred to a maternal-foetal medicine (MFM) specialist for counselling and advice. The O&G doctor may recommend regular ultrasounds to monitor for foetal growth and abnormalities. MOH will also arrange for her to be admitted to a public hospital for further management and care if necessary.
10. Amniotic fluid testing for Zika may be offered to the pregnant woman after 15 weeks of pregnancy. However as there is currently not enough research to ascertain the effectiveness of testing for Zika in amniotic fluid, a positive Zika test in amniotic fluid does not always mean that the foetus will have birth defects.
11. It is important to note that a positive Zika test does not mean that the foetus is infected or harmed. Depending on the population studied and the research methodology, the estimated risk of microcephaly associated with Zika virus infection during pregnancy can vary widely. A recent study published in the New England Journal of Medicine found that the risk of an infected mother giving birth to a child with microcephaly is between one to 13 percent.[2]
Prevention of Infection
12. Prevention of Zika virus infection is the best protection for both the pregnant woman and her foetus. We advise pregnant women to undertake strict precautions against mosquito bites and seek medical attention immediately if they become symptomatic. Although Zika virus infection remains a predominantly vector-borne disease, a small number of cases of sexual transmission have been documented. Potentially exposed males with female partners who are pregnant should practise safe sex through the correct and consistent use of condoms, or abstinence, for the duration of their female partner’s pregnancy.
13. Women with confirmed Zika virus infection should abstain from sexual intercourse for at least eight weeks after recovery. Men with confirmed Zika virus infection but whose female partner is not pregnant should also adopt safe sexual practices, e.g. consistent and correct use of condoms during sex, or consider abstinence for six months after recovery.
14. Pregnant women who are concerned about their pregnancy should consult their doctor for advice.
______________________________________________________________________
FREQUENTLY ASKED QUESTIONS ON ZIKA AND PREGNANCY
FOR COUPLES PLANNING PREGNANCY
1. If a woman who is not pregnant is bitten by a mosquito and infected with Zika virus, will her future pregnancies be at risk?
Zika virus infection does not pose a risk of birth defects for future pregnancies.
2. If a couple is planning for pregnancy, what is MOH’s advice if either one lives, works or studies in an affected area?
If both the man and woman are well
They should take strict precautions against mosquito bites, and if they have further questions, consult their doctor.
If woman is symptomatic
(with fever and rash and other symptoms such as red eyes or joint pain)
She should seek medical attention promptly, and if confirmed positive for Zika, she should practise safer sexual practices or abstain from sexual intercourse for at least 8 weeks after recovery, before trying to conceive.
If the man is symptomatic
(with fever and rash and other symptoms such as red eyes or joint pain)
He should seek medical attention promptly, and if confirmed positive for Zika, he should practise safer sex through the correct and consistent use of condoms or abstain from sexual intercourse for at least six months after recovery.
FOR PREGNANT WOMEN AND THEIR PARTNERS
Testing and Prevention
1. Are there any tests which can be done to determine if a pregnant woman is infected with Zika?
Currently, the only reliable test available for Zika is the reverse transcriptase-polymerase chain reaction (RT-PCR) test which looks for genetic material of the virus in blood or urine. However, RT-PCR test is only able to detect Zika infection in blood within 5-7 days of onset of symptoms and in urine within 14 days of onset. Therefore, the time window in which a pregnant woman can be tested using RT-PCR is very short.
At present, there is no reliable serological test (which looks for antibodies in the blood) for Zika.
2. If I am pregnant and my male partner is tested positive for Zika, do I need to get tested if I do not have any symptoms?
If you have had sexual intercourse with your partner, you should consult a doctor and inform him/her of possible exposure to Zika so that he/she can arrange for Zika testing.
3. If I am pregnant and asymptomatic, but worried about possible exposure to Zika, where should I go to get tested?
WHO's May 2016 guidelines and MOH's August 2016 clinical guidelines on Zika virus infection and pregnancy do not recommend routine Zika testing for asymptomatic pregnant women. If you are concerned, you should discuss further with your doctor.
4. Should a woman who is pregnant get regular blood/ urine tests for Zika, to make sure that she is not infected?
No, unless she has symptoms of possible Zika Virus Infection (fever and rash and other symptoms such as red eyes or joint pain).
5. Is it safe for pregnant women to use insect repellent?
Yes, insect repellents sold in Singapore are safe for use for pregnant women.
You can also prevent mosquito bites by wearing long, covered clothing, and sleeping under mosquito nets or in rooms with wire-mesh screens or air-conditioned rooms to keep out mosquitoes.
6. If I am pregnant and have recently visited a Zika affected area in Singapore, what should I do?
There is no need to see your doctor, if you are well. You should continue to take strict precautions against mosquito bites. If you have symptoms of possible Zika virus infection (fever and rash and other symptoms such as red eyes or joint pain), you should seek medical attention immediately, and consult your Obstetrics and Gynecology (O&G) doctor.
7. If I am pregnant and live, work or study in a Zika affected area in Singapore, what should I do?
You should take steps to prevent mosquito bites and consult a doctor if you develop a fever and rash and other symptoms such as red eyes or joint pain after possible exposure to Zika. You should tell the doctor where you live, work or study.
8. If my female partner is pregnant and I am tested positive for Zika, what should I do?
You should practise safe sex through the correct and consistent use of condoms, or abstinence, for at least the whole duration of your female partner’s pregnancy.
9. If my female partner is pregnant and I live, work or study in a Zika affected area in Singapore, what should I do?
You should practise safer sex through the correct and consistent use of condoms, or abstinence, for at least the whole duration of your female partner’s pregnancy.
You should take steps to prevent mosquito bites by wearing long, covered clothing, applying insect-repellent, and sleeping under mosquito nets or in rooms with wire-mesh screens or air-conditioned rooms to keep out mosquitoes.
You should consult a doctor if you develop a fever and rash and other symptoms such as red eyes or joint pain after possible exposure to Zika. You should tell the doctor where you live, work or study.
Pregnant women/ Mothers with Zika
1. What is being done in other countries to manage pregnant women with Zika? Is Singapore doing the same?
In countries with community transmission of Zika Virus Infection and in line with WHO’s guidelines, pregnant women with Zika are advised to follow up closely with healthcare practitioners to detect any fetal abnormalities. Singapore has also adopted similar recommendations.
2. If I am pregnant and my blood tests positive for Zika, will I need to be hospitalised?
Like other patients tested positive for Zika, you should be referred to a hospital and managed by an O&G doctor.
3. If I am pregnant and positive for Zika Virus Infection, will my baby have microcephaly?
Currently, even if a pregnant woman is confirmed to be infected with Zika virus, there is no test that will predict the future occurrence of microcephaly. We advise that you follow-up closely with your doctor.
4. If a pregnant woman is positive for Zika virus Infection, should she consider termination of pregnancy?
A pregnant patient with confirmed Zika infection will be arranged for admission to a public hospital with a referral to an O&G doctor for further management. Serial ultrasounds and amniotic fluid testing may be considered after the potential risks and interpretation of results are discussed. The termination of pregnancy is a personal choice which should be carefully made by the parents in consultation with their doctor.
5. Can mothers with Zika infection breastfeed their baby?
Zika virus has been detected in breast milk but there is currently no evidence that the virus is transmitted to babies through breastfeeding.
QUESTIONS ON ZIKA VIRUS AND MICROCEPHALY
1. What is Microcephaly?
Microcephaly is a congenital condition in which the head size is very much smaller than usual for a baby of the same age, race, and sex.
Microcephaly can be caused by a variety of genetic and environmental factors, such as Down Syndrome, exposure to drugs, alcohol or other toxins in the womb; rubella and a few other infections during pregnancy.
There is no specific treatment for this condition. Infants with microcephaly showing developmental delay might benefit from early intervention programs or developmental, physical, and occupational therapy, as well as interdisciplinary programmes.
2. Does Zika cause microcephaly?
There is evidence that Zika can cause microcephaly.
3. What is the impact of microcephaly on an infant?
Microcephaly can be an isolated condition, meaning that it can occur with no other major birth defects, or it can occur in combination with other birth defects. Infants with microcephaly may have concurrent disabilities. Different symptoms and signals associated with microcephaly (very small head, difficulty feeding, high pitched crying, fits, stiffness of arms and legs, developmental delays and disabilities, among others) have been described.
Infants with suspected microcephaly should be evaluated by a healthcare professional. In addition to clinical evaluation, neuroimaging tests to evaluate possible structural deformities may be required.
4. Can microcephaly be picked up through pre-natal screening? If so, what options are available to pregnant women if it is detected?
Microcephaly may be picked up during pre-natal screening, such as through ultrasound of the fetus. However, not all cases may be picked up in the early stages of pregnancy (i.e. within the first trimester). Some may not be diagnosed until after late in the pregnancy or after the birth of the child. This is similar to other congenital conditions, such as Down Syndrome. Similarly, a small head measured on ultrasound does not necessarily confirm the diagnosis of microcephaly. A significant proportion of fetuses with small heads on ultrasound turn out to be neuro-developmentally normal.
If this condition is picked up through pre-natal screening, the parents should consult with their healthcare professional on their options.
5. Can amniocentesis tests be used to detect Zika Virus Infection in the fetus?
If the woman is not known to be infected with Zika virus, amniocentesis is not recommended for detecting Zika virus infection in the fetus. If the woman is confirmed to be positive for Zika, the O&G doctor will assess and counsel her on the pros and cons of doing such a test.
6. I think my child’s head is smaller than usual. Does he have microcephaly?
Having a seemingly smaller head may not mean that your child has microcephaly. Just as importantly, having a small head does not automatically mean that the child will have developmental concerns. The child should be evaluated by a healthcare professional. More tests may be needed to determine if there are any issues of concern.
7. Can microcephaly be treated? What support can be provided to a child born with microcephaly?
Treatment and support depend on whether the child has any disabilities and if so, the type and degree of disability. Treatment and support will include rehabilitative measures which may include environmental stimulation, physiotherapy, speech therapy and occupational therapy.
Subscribe to receive newsletter on pregnancy and parenting in Singapore.