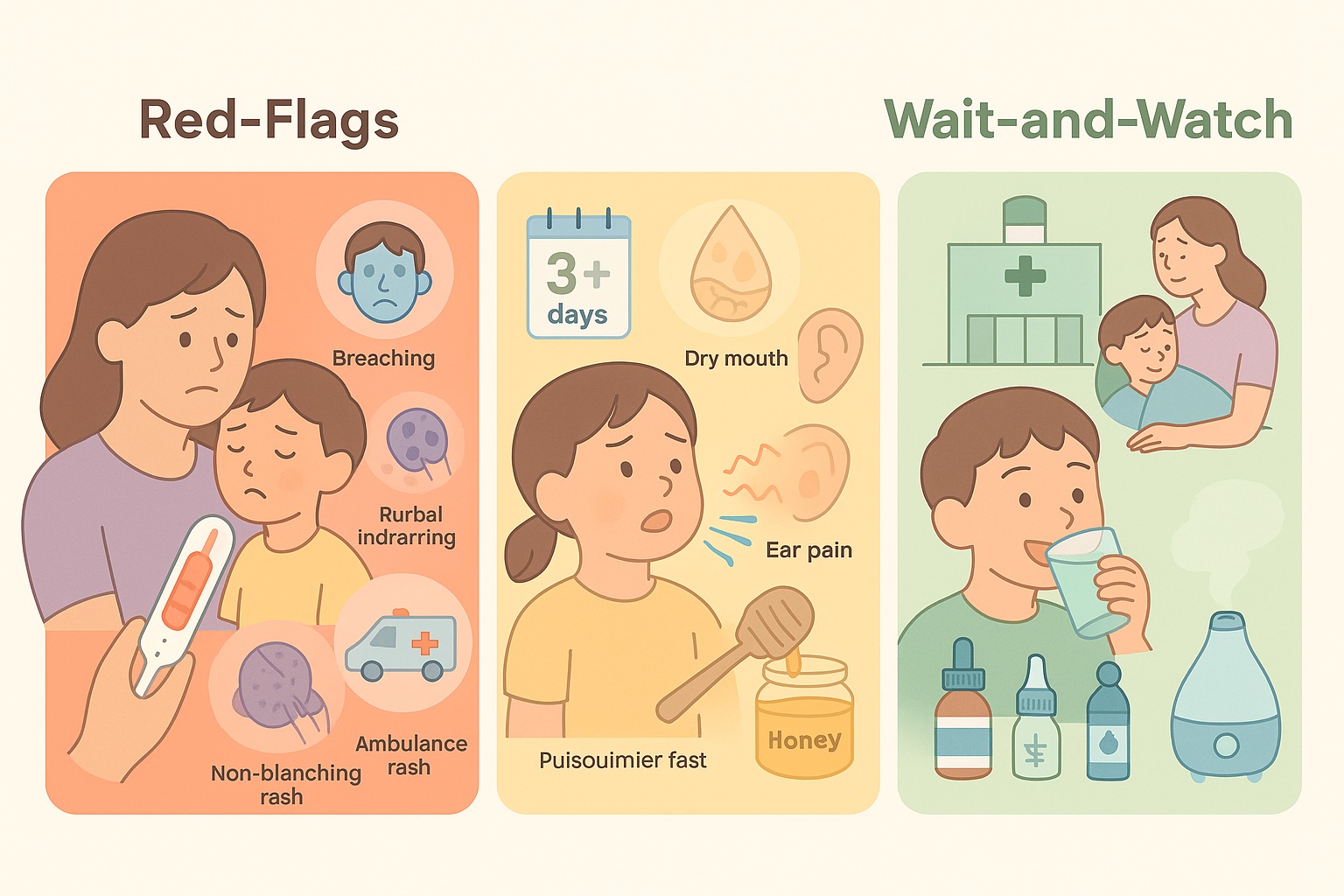
Fever, Cough & Runny Nose in Kids: Red Flags vs. Wait andWatch
Clear, evidence-based thresholds for when to go to the emergency department, see a doctor the same day, or care for your child at home.
1) Go to A&E RED FLAGS
- Very hard to wake, floppy, or looks seriously unwell; weak/high-pitched continuous cry.
- Breathing danger signs: grunting, severe chest indrawing, or very fast breathing (see table). Stridor/noisy breathing at rest.
- Blue/grey/pale skin or lips.
- Non-blanching purplish rash (pressing a glass does not make it fade).
- Seizure or confusion.
- Infants < 3 months with temperature more than or equal to 38.0 °C (any fever in this age group).
2) See a clinic the same day AMBER
- Breathing concerns without the red-flag features: nasal flaring, crackles, or fast breathing above age thresholds; home pulse oximeter less than 95% on room air.
- Age 3–6 months with temperature more than or equal to 39.0 °C.
- Signs of dehydration: very dry mouth, fewer wet nappies/urine, poor drinking, capillary refill more than or equal to 3 s.
- Fever persisting > 3 days (older infants/children), or fever that improves then returns.
- Ear pain with fever, ear discharge, or symptoms lasting > 48–72 hours.
- Fever for 5 days or more (your doctor may consider Kawasaki disease, especially with red eyes, cracked lips/strawberry tongue, swollen hands/feet or rash).
3) Safe to “wait & watch” at home GREEN
- Child is alert, breathing comfortably, drinking and urinating normally, and has no red/amber signs.
What helps
- Fluids & rest; light clothing. Check through the night.
- Paracetamol or ibuprofen for discomfort (weight-based dosing; ibuprofen usually for children older than 6 months). Use only while the child appears distressed—don’t alternate routinely.
- Honey ½–1 tsp at bedtime may ease cough in children aged 1 year and up.
- Saline nose drops/spray for congestion; cool-mist humidifier if helpful.
What to avoid
- OTC cough/cold syrups in very young children (limited benefit, potential harms). Seek professional advice for < 2 years; avoid products containing codeine in children.
- Tepid sponging (not recommended for fever management).
- Honey in infants < 1 year (risk of infant botulism).
Age-specific breathing thresholds
| Age | “Fast” breathing | Action |
|---|---|---|
| < 6 months | > 60 breaths/min | RED (seek urgent care) |
| 6–12 months | > 50 breaths/min | AMBER (same-day clinic) |
| > 12 months | > 40 breaths/min | AMBER (same-day clinic) |
Count for 60 seconds while the child is calm. If you use a home oximeter, SpO2 less than 95% on room air is concerning—seek same-day care.
Runny nose: myth-busting
Green/yellow snot is not equal to automatic antibiotics. Colour alone cannot distinguish viral from bacterial infection. Seek care if symptoms are severe, worsening, or persist > 10 days (or “double-sickening”).
How long should a cough last?
A typical viral cough can linger for 2–3 weeks. See your doctor if cough lasts > 4 weeks, or earlier if breathing becomes hard, there is stridor, wheeze, or the child looks unwell.
Quick medication notes (Singapore-relevant)
- Paracetamol: dose by weight (commonly 10–15 mg/kg per dose every 4–6 hours; max 4 doses/day). Follow your product’s label.
- Ibuprofen: generally for children older than 6 months; dose by weight as per label. Avoid if dehydrated or if advised by a doctor.
Always read the label; check with your GP/pharmacist for age/weight-specific dosing and if your child has chronic conditions.
Singapore quick links
It takes a village to raise a child !
Join our WhatsApp Groups or Facebook Group to interact with parents about infant care/child care in Singapore..